The following tables contain dosages for medicines used in treatment of uncomplicated malaria.
Dosage of artemether/lumefantrine 20/120 mg
|
WEIGHT (KG)
|
DAY 1
|
DAY 2
|
DAY 3
|
|
<14
|
1 tablet at 0 hours
then 1 tablet at 8 hours
|
1 tab twice daily
|
1 tab twice daily
|
|
15–24
|
2 tablets at 0 hours,
then, 2 tablets at 8 hours
|
2 tab twice daily
|
2 tab twice daily
|
|
25–34
|
3 tablets at 0 hours then 3 tablets at 8hours
|
3 tab twice daily
|
3 tab twice daily
|
|
>35
|
4 tablets at 0 hours
then 4 tablets at 8 hours
|
4 tab twice daily
|
4 tab twice daily
|
|
Note: Give day 2 and day 3 doses every 12 hours
|
Dosage of artesunate (AS) tablets 50 mg once a day
|
AGE
|
DAY 1
|
DAY 2
|
DAY 3
|
|
0–11
months
|
25 mg (½ tab)
|
25 mg (½ tab)
|
25 mg (½ tab)
|
|
1–6 years
|
50 mg
(1 tab)
|
50 mg
(1 tab)
|
50 mg
(1 tab)
|
|
7–13 years
|
100 mg
(2 tabs)
|
100 mg
(2 tabs)
|
100 mg
(2 tabs)
|
|
>13 years
|
200 mg
(4 tabs)
|
200 mg
(4 tabs)
|
200 mg
(4 tabs)
|
|
Note: Do not use artesunate alone, give with amodiaquine tabs
|
Dosage of amodiaquine (AQ) 153 mg tablets
|
AGE
|
DAY 1
|
DAY 2
|
DAY 3
|
|
0–11
months
|
76 mg (1/2 tab)
|
76 mg (1/2 tab)
|
76 mg (1/2 tab)
|
|
1–6 years
|
153 mg (1 tab)
|
153 mg (1 tab)
|
153 mg (1tab)
|
|
7–13 years
|
306 mg (2 tabs)
|
306 mg (2 tabs)
|
306 mg (2 tabs)
|
|
>13 years
|
612 mg (4 tabs)
|
612 mg (4 tabs)
|
612 mg (4 tabs)
|
|
Note: Do not use amodiaquine alone, use with artesunate tabs
|
Dosage of dihydroartemisinin (DHA)/Piperaquine tablets (PPQ) (40/320 mg) tablets
|
WEIGHT (KG)
|
AGE
|
DAY 1
|
DAY 2
|
DAY 3
|
|
<5–9.9
|
<6 month– 1 year
|
0.5
|
0.5
|
0.5
|
|
10–20
|
2–7 years
|
1
|
1
|
1
|
|
20-40
|
8-13 years
|
2
|
2
|
2
|
|
40-60
|
|
3
|
3
|
3
|
|
60-80
|
|
4
|
4
|
4
|
|
>80
|
|
5
|
5
|
5
|
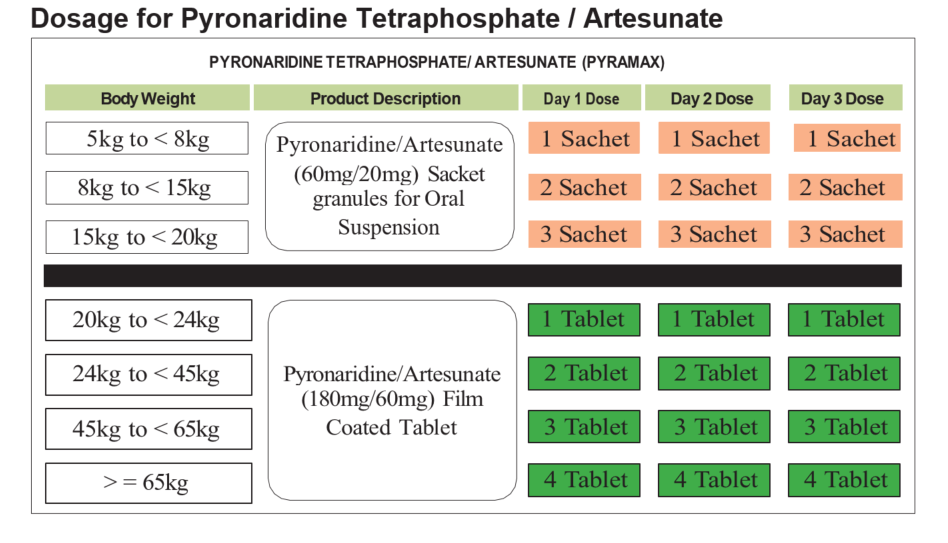
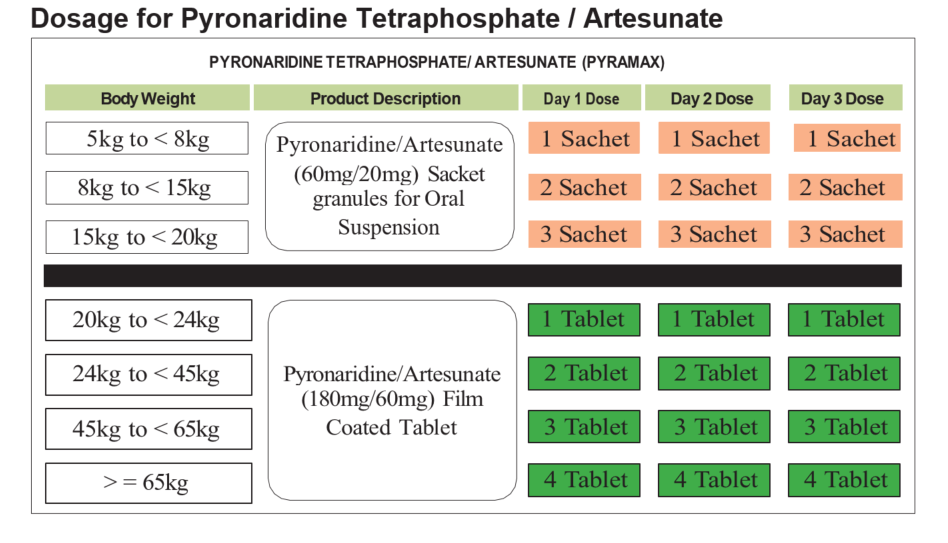
Dosage for Pyronaridine Tetraphosphate / Artesunate
Dosage of quinine tablets (1 quinine tab=300 mg salt)
|
WEIGHT (KG)
|
AGE
|
DOSE (TO BE GIVEN EVERY 8 HOURS FOR 7 DAYS)
|
|
<5–10
|
3 months–1 year
|
75 mg ( tab)
|
|
10–18
|
1–5 years
|
150 mg (½ tab)
|
|
18–24
|
5–7 years
|
225 mg ( tab)
|
|
24–30
|
7–10 years
|
300 mg (1 tab)
|
|
30–40
|
10–13 years
|
375 mg (1 tab)
|
|
40–50
|
13–15 years
|
450 mg (1½ tab)
|
|
> 50
|
> 15 years
|
600 (2 tabs)
|