Pneumonia
exp date isn't null, but text field is
Introduction
An inflammation of the lung parenchyma
Various bacterial species, fungi and viruses may cause pneumonia. The setting in which infection is acquired could be a predictor of the infecting pathogen
Bacterial Pneumonia: is defined as bacterial infection of the lung parenchyma associated with recently developed radiological shadowing which may be segmental, lobar or multi lobar.
Types
- Community Acquired Pneumonia (CAP)
- Hospital Acquired pneumonia (HAP)
- Ventilator Associated pneumonia (VAP)
- Health care associated Pneumonia (HCAP)
- Pneumonia in the immunocompromised
- Aspiration pneumonia
Common bacteria causing CAP:
- Streptococcus pneumonia (Most common cause)
- Mycoplasma pneumonia
- Legionella pneumophilia
- Chlamydia pneumonia
- Haemophilus influenza
- Staphylococcus aureus
- Chlamydia psittaci
- Coxiella burnetti
- Klebsiella pneumonia
- Actinomyces israelli
- Haemophilus influenzae
- Pseudomonas aeruginosa (usually implicated in nosocomial pneumonia)
Clinical Features
Typical pneumonia:
- Sudden onset fever, chills and rigors
- Cough with purulent sputum production
- Pleuritic chest pain
- Breathlessness with short inspiratory efforts
Signs:
- Fever
- Herpes labialis
- Tachypnoea
Signs of lung consolidation:
- Pleural friction rubs
- Chest signs are very helpful depending on the phase of the inflammatory response
- Dull percussion
- Increased tactile and vocal fremitus
- Bronchial breath sounds
- Whispering pectoriloquy
- Crepitations
Signs of severity:
- Confusion
- Urea > 7mmol/L
- Respiratory rate > 30/min
- Systolic BP <90
- Age < 65years
- In Children: inability to feed or drink, cyanosis, alteration in level of consciousness
Score 1 point for any of the above features present
- 0 or 1- home treatment
- 2 - Hospital-supervised treatment
- 3 or more- manage in Hospital as severe pneumonia
- 4 or 5 — ICU Admission
Atypical pneumonia:
- Gradual onset
- Dry cough
- Prominent extra-pulmonary symptoms
- Headache
- Sore throat
- Fatigue
- Myalgia
- Chest crackles or rales
Differential Diagnoses
- Acute bronchitis
- COPD Exacerbation
- Pulmonary embolism/infarction
- TB
- Pulmonary eosinophilia
Complications
- Empyema thoracis
- Pleural effusion
- Lung abscess
- Lobar collapse
- Deep vein thrombosis and pulmonary embolism
- Pneumothorax
- ARDS
- Multi organ failure
- Hepatitis, pericarditis, myocarditis, meningoencephalitis
- Pyrexia from drug hypersensitivity
Investigations
- FBC +ESR+ CRP
- Serum Electrolyte, Urea and Creatinine
- LFT
- Blood Culture
- Serology
- Cold agglutinins
- Arterial blood gases/ SPQ
- Sputum gram stain, M/C/S
- Urine pneumococcal and legionella antigen
- Chest X-ray
- Pleural fluid M/C/S
Treatment Goals
- Eliminate the infection
- Return to normal lung function
Drug Treatment
General
- Oxygen to maintain PaO2 at or above 8kPa
- IV fluids especially in severe cases
- Antipyretics
- Antibiotics
Uncomplicated CAP and No modifying factor, no antibiotics use in the last 3 months:
Co-amoxiclav
- Adult: 1 g 12 hourly for 5 — 7 days
- Child:
- Neonate and premature infants, 25 mg/kg/dose 12 hourly
- Infants up to 3 months, 25 mg/kg/dose 8 hourly
- 3 months — 12 years, 25 mg/kg/dose 8 hourly increased to 6 hourly in more severe infections
Or
Benzyl penicillin
- Adult: initially 2 million units 6 hourly
- Child:
- preterm and neonate under 7 days, 25 mg/kg by IM injection Or by slow IV injection or infusion every 12 hours; double dose in severe infections
- Neonate 7 — 28 days: 25 mg/kg 8 hourly; double dose in severe infections
- 1 month — 18 years: 25 mg/kg, 4 — 6 hourly; Double dose in severe infections
Commence oral therapy as soon as possible
Or
Macrolide (azithromycin 500 mg stat, then 250 mg daily, or clarithromycin 500 mg twice daily for up to 14 days)
Or
Cefuroxime axetil
- Adult :500 mg orally 8 hourly for 5 — 7 days
- Child:
- 3 months — 2 years 10 mg/kg (maximum 125 mg) orally 12 hourly
- 2 —12 years 15 mg/kg orally 12 hourly
- 12 — 18 years 12 hourly; May double doses in severe infections.
Fourth generation Cephalosporins:
Cefpodoxime
- Adult: 200 mg orally 12 hourly
- Children: 4 mg/kg/dose orally 12 hourly
Patients with history of recent use of Antibiotics:
- Respiratory quinolone (levofloxacin). Quinolones are generally better avoided in TB endemic areas because of their potential use as part of 2 line regimen in the treatment of MDR-TB.
- Advanced macrolide plus amoxycillin
- Advanced macrolide plus amoxycillin+clavulanic acid
Complicated CAP
- IV B lactam plus advanced macrolide
- IV respiratory quinolones plus advanced macrolide
- Penicillin G+advanced macrolide
- Consider Pneumocystis jiroveci in HIV patients: Co-trimoxazole
Notable Adverse Drug Reaction, Contraindications and Caution
- Co-amoxiclav: Nausea, diarrhoea, skin rashes, contraindicated in penicillin hypersensitive individuals
Cefuroxime: Nausea, vomiting, abdominal discomfort, headaches, rarely antibiotic associated colitis
Macrolides: Similar to those mentioned above but usually milder. Hepatotoxicity and antibiotic associated colitis are quite rare
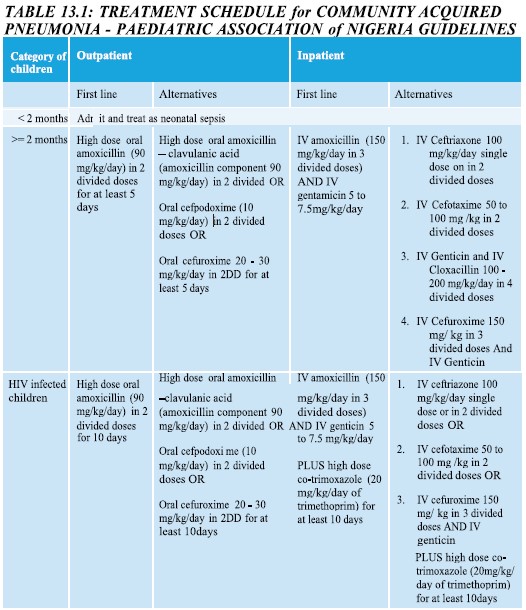
Table:
Prevention
- Pneumococcal vaccine
- Haemophilus influenzae vaccine
