Burns
exp date isn't null, but text field is
EMERGENCY MANAGEMENT OF BURNS: ADULTS
- Remember the ABCs of life support
- If evidence of inhalation, such as singed nasal hairs, soot in nose, refer to tertiary hospital
- Pain relief (refer to Palliative Care section)
- Assess the severity of the burn (see tables below)
- Refer patients with burns of more than 15% of body surface area (BSA) to hospital on IV fluid therapy for resuscitation and burns dressing
Refer all deep burns or burns of the face, neck or hands and perineum for further assessment
Burns across joints should be immobilized and later encourage passive movement to prevent from contractures
- If the burn is more than 40%,
- mortality is almost 100% therefore referral to a tertiary hospital may not be necessary
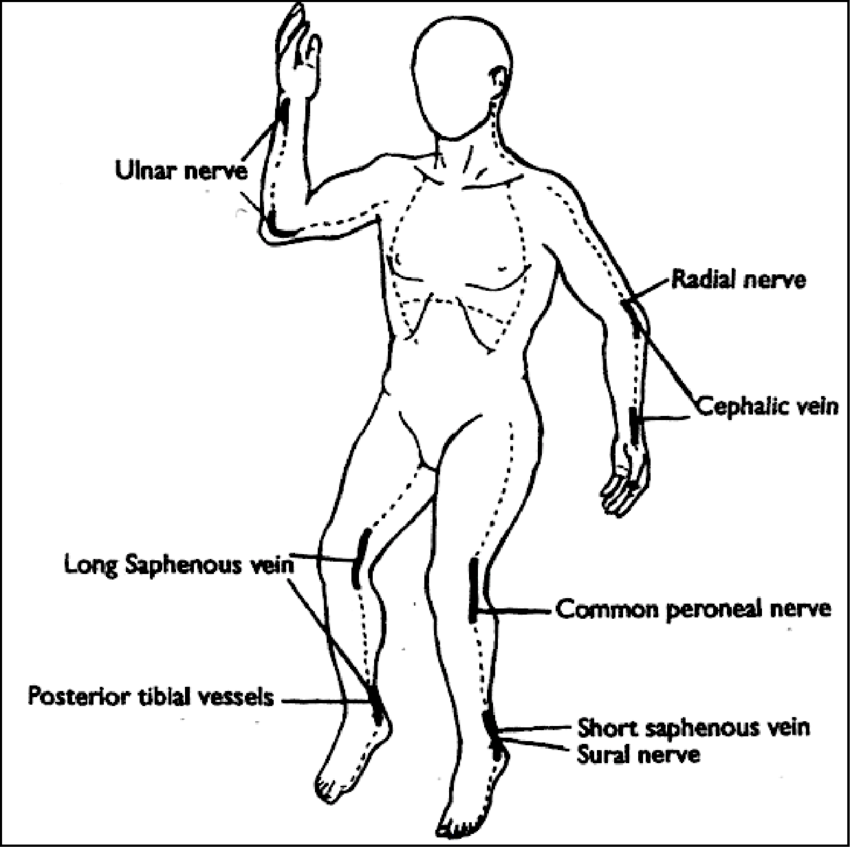
- Circumferential burns of the limbs and trunk require immediate bed side escharotomy (see diagram of the site of incisions)
Burns by nature are usually initially sterile

Treatment
- The Aim of treatment is to speed healing while minimizing the risk of infection
- In the sick burned patient (fever + diarrhoea+/- a rash):
- Have a high index of suspicion of toxic shock syndrome
- Nasogastric tube insertion is helpful as gastric dilatation is common
- Give anti-acids to prevent gastric stress ulcers
- Do a blood culture and material parasites
- Start intravenous Flucloxacillin 1g IV 6 hourly for 5 days
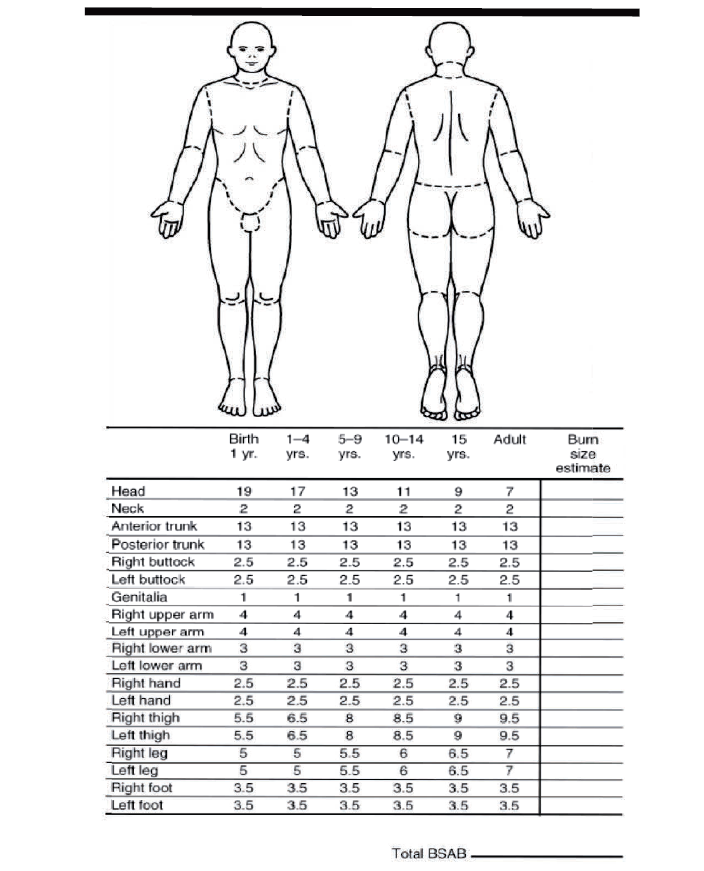
- Calculation of Body Surface Area Affected
Adults
- Give IV fluid replacement according to the calculation below
- With mild burns (< 15% adults BSA burned) give oral fluid replacement therapy using as much ORS as the patient will tolerate
Adults
- With 15% or more require IV fluid resuscitation
- Calculate according to Parkland formula: - Adults: 4mls per /kg body weight/ TBSA
CALCULATION OF IV FLUID REPLACEMENT
The object is to maintain normal physiology as reflected by urine, vital signs and mental status
Use Ringer's Lactate IV infusion or (if this is not available) Normal Saline
A general formula and dosage schedule that may be used for the first 24 hours is:
- Total volume of IV infusion required (before above additions) = 4 ml/kg x % BSA burned plus normal daily requirement
- Give 50% of this total in the first 8 hours calculated from the time of burn
- Give 50% in the next 16 hours
- Give analgesic treatment
- Strong analgesia (e.g., Morphine or Pethidine) will be required for the first 48 hours

EMERGENCY MANAGEMENT OF BURNS: CHILDREN
- Assess the patient using the cAcBcDE approach to identify and manage any life-threatening injuries.
- Assess the % total body surface area using the paediatric Lund-Browder Chart, the palmar surface of the patient’s hand or the Wallace’s rule of nines chart (as adapted for children).
- Assess the depth of burns.
Treatment
- If there is evidence of an inhalational injury:
- Discuss with paediatric ICU or anaesthesia,
- Early intubation is imperative.
- Refer and transfer safely to a burns unit.
- Children with extensive burns must be given oxygen.
- Those with severe respiratory distress may require intubation and ventilation.
- Circumferential full-thickness burns require urgent escharotomy. Keep patients warm.
- Ensure adequate analgesia is given.
- Prophylactic antibiotics are not recommended.
Fluid management
- Children with shock require fluid resuscitation using 10ml/kg over 20 minutes.
- Note: children with burns rarely present with shock, so a careful assessment should be made to identify the underlying cause of the shock.
- Children with ≥10% TBSA burns need additional intravenous fluid therapy.
- This fluid requirement is calculated from the time of injury using the Parkland formula: Total fluid replacement for burn in 24 hours (mls) = 4 mls x %TBSA x weight (kg)
- Half this fluid is given within the first 8 hours from the time of the burn. The rest is given over the following 16 hours.
- The child should also receive maintenance fluids, which must contain at least 5% dextrose.
- Patients should be catheterised as urine output guides ongoing fluid requirements.
- Adequate nutrition is crucial for management of burns patients.
- Children with burn injuries >10% TBSA need supplemental nutrition to aid recovery.
Toxic shock syndrome
- Occurs within 48 hours of injury,
- Suspected in children with relatively small burns and fever, rash, and/or vomiting and diarrhoea.
- This is an emergency.
- Management includes:
- Oxygen
- If in shock: 10 ml/kg of ringer’s lactate or 0.9% saline over 1 hour
- Antibiotics: flucloxacillin or ceftriaxone
- Antipyretics: paracetamol
- Strict fluid balance
Referral
- Children who require referral and transfer to a burns unit
Note: always consider the possibility of child abuse in burn injuries
BURNS WOUND MANAGEMENT
Under aseptic conditions, gently cleanse the lesion with Cetrimide 15% + Chlorhexidine 1.5% diluted 1 part in 20 parts water.
Alternative:
- Cleanse with Hydrogen Peroxide Solution 3% or soap and water
- Never use alcohol-based solutions
- Repeat the cleansing each day debriding the lesion and removing necrotic tissue as necessary
- Give tetanus toxoid vaccination (see Section 12.3) If patient is developing signs of tetanus
- Give Tetanus Antitoxin (ATS) 1,500 units s/c or IM
Once the lesion is clean/clear of necrotic tissue:
- Refer for skin grafting, if necessary, otherwise
- Dress the burn with Paraffin Gauze Dressing
- Cover this with dry gauze dressing thick enough to prevent seepage through to the outer layers
- Change the dressing after 2-3 days, and then as necessary
If the burn becomes infected:
Apply Silver Sulphadiazine Cream 1% bd
- Before application, completely remove any old topical medication
- Cover with sterile gauze
If the patient becomes ill after burn infection:
- Carry out culture and sensitivity testing on the exudates
- Treat with systemic antibiotic(s) according to findings
