Asthma (Recurrent Wheezing)
exp date isn't null, but text field is
CLINICAL DESCRIPTION
Asthma is chronic inflammatory airway disease characterized by recurrent reversible airway obstruction, increased responsiveness of bronchial tree to a variety of stimuli resulting into recurrent episodes of wheezing, cough, chest tightness and shortness of breath. Triggers include house dust mite, fumes, perfumes, pollen, infection, pets hair, smoke, air pollution, emotions, infection, exercise, drugs (e.g., Aspirin/NSAIDs, beta-blockers such as propranolol), food (e.g. milk, peanut, egg, fish, wheat), weather change etc.
Asthma Phenotypes:
- Allergic asthma phenotype: easy to recognize and begins in childhood.
- Associated with a past and/or family history of allergic disease such as eczema, allergic rhinitis, conjunctivitis or food or drug allergy. Eosinophilic inflammation and respond well to inhaled corticosteroid (ICS) treatment.
- Non-allergic phenotype: in some adults and have neutrophilic or eosinophilic inflammation and may respond less to inhaled corticosteroid
- Occupation related asthma: symptoms may be triggered by work environment exposures
- Asthma with fixed airway obstruction: long-standing asthma develop fixed airflow limitation due to airway wall remodeling.
- Asthma with obesity: some obese asthma patients have little eosinophilic airway inflammation
- Exercise induced asthma: some patients/athletes have asthma symptoms during or after exercise
CLINICAL FEATURESSIGNS AND SYMPTOMS
- Wheezing
- Chest tightness/breathlessness
- Coughing
- Nasal polyp and eczema (in some allergic asthma patients)
- Wheezes and respiratory distress (if during attack)
- May have normal physical examination (in between asthma attacks)
INVESTIGATIONS
- Asthma diagnosis is mainly based on classical recurrent nocturnal and daytime respiratory symptoms +/-wheezes on physical examination.
- Full blood count: mildly high eosinophil count in allergic asthma phenotype
- In some central/private hospitals: high total IgE (in allergic asthma)
- Spirometry: Reduced FEV1, FEV1/FVC <70% with reversible obstruction (increase in FEV1 by 200ml and 12% post-bronchodilator).
Note: Patient with long standing uncontrolled asthma may develop irreversible airway obstruction due to airway remodeling. Spirometry can be normal in asthma between attacks.
- Peak Expiratory Flow Rate: reduced for expected value (for age, sex and height) and excessive diurnal variability of >10% in adults and >13% in children on twice daily measurement of PEFR
- CXR only to exclude complications of asthma (e.g., pneumothorax/pneumomediastinum, pneumonia) or other pathologies
- Stool analysis (to exclude helminths ova)
Beware of mimics of asthma
- Anaphylaxis reaction
- Heart failure causing cardiac asthma due to pulmonary edema
- COPD
- Helminthiasis (Loeffler syndrome)
- Upper-airway obstruction (stridor main feature)
- Vocal cord dysfunction syndrome (paradoxical adduction of vocal cords in inspiration in people with psychological stresses. Diagnosis is through direct laryngoscopy to confirm the paradoxical adduction of vocal cords during inspiration)
COMPLICATIONS OF ASTHMA
- Recurrent acute exacerbations (attacks).
- Pneumothorax/Pneumomediastinum/surgical emphysema (if in severe attack).
- Respiratory failure (in severe attack)
- Pneumonia risk
ACUTE ASTHMATIC ATTACK (ACUTE EXACERBATION)
Can be mild, moderate, severe or life threatening
TREATMENTTREATMEN OBJECTIVES
- Relieve symptoms of bronchoconstriction with bronchodilators.
- Control airway inflammation with inhaled steroid (very important).
- Prevent further acute attacks and complications.
- Educate patients to avoid triggers where possible.
- Educate patient- good inhaler or spacer use technique and assess at every clinic visit.
- Monitor asthma treatment side effects and address appropriately.
- Assess and address patient fears/myths.
- Assess asthma control at each visit and adjust treatment accordingly

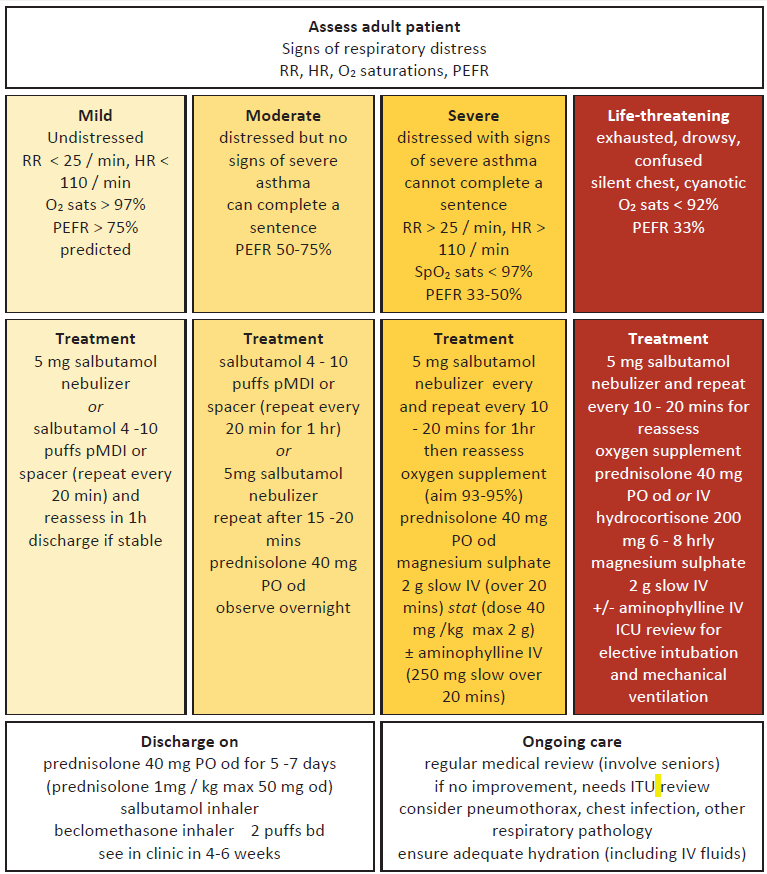
Notes: during asthmatic attack
- Can use plastic bottle as a spacer for inhalers
- Systemic steroids (oral prednisone or IV hydrocortisone) are VERY important: exacerbation= inflammation. Give within 1hour of patient arrival to hospital as it takes about 4 hours for the steroids to start working
- Magnesium sulphate IV 1.2 -2 g stat (40 mg / kg, max 2 g) (dilute in saline and infusion over 20 minutes): mode of action: bronchodilator and anti-inflammatory. Side effects: hypotension and respiratory depression (rare). Contra-indicated in severe renal failure (creatinine clearance < 30 ml / min), AV block, myocardial disease, myasthenia gravis.
- Give IV aminophylline slowly and watch for toxicity (arrhythmias and seizures). Dosage: IV Aminophylline 250 IV slow push over 20minutes or 250 - 500mg as IV infusion in 1L of 5% Dextrose or 0.9% Sodium Chloride over 12 hours. Where possible IV aminophylline should be given when patient has not responded to salbutamol nebulization and magnesium sulphate
- If no response to above medication can give Adrenaline 0.5-1.0ml of 1:1000 slowly nebulized or IM
- When patient is already on maintenance oral Aminophylline avoid giving loading dose of IV Aminophylline
- Antibiotic only indicated if patient has signs of pneumonia
- Salbutamol tablets not ideal for asthmatic attack/asthma maintenance therapy (poor bioavailability and high risk of side effects e.g., heart palpitation/tremor). Salbutamol inhaler preferred.
- If patient asthmatic attack not improving consider escalating treatment facility level, exclude pneumothorax, mimics of asthmatic attack (e.g., Pulmonary embolism, pulmonary edema)
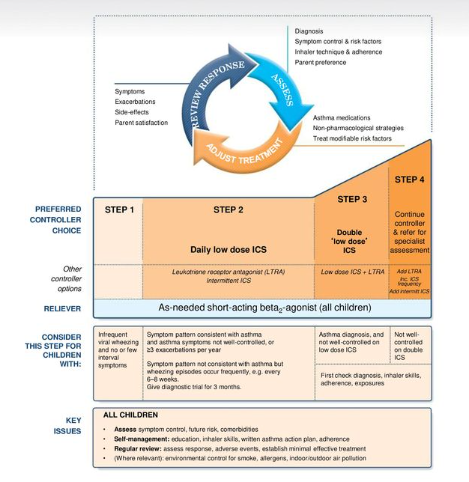
MAINTENANCE AND PREVENTIVE TREATMENT OF ASTHMA - THE STEPWISE APPROACH
- An environment free from cigarette and wood smoke can reduce attacks
- Check compliance and inhaler technique at each step before progressing
- Step up where required due to frequency of exacerbations
- Step down where possible:
- STEP 1: if symptoms less than twice a week Initial treatment should be with Salbutamol inhaled via a spacer device (see above) as required
- STEP 2: If symptoms more than twice a week add preventive therapyinhaled steroid e.g. Beclomethasone 2 puffs (200mcg) 12 hourly via a spacer. Increasing to 4 puffs twice a day as required.
- STEP 3: Refer for specialist care if no control with steps 1 & 2
Alternatively (to be used only if the above are NOT available)
- Give Aminophylline 100mg 12 hourly or 8 hourly.
ASTHMA IN CHILDREN
- Episodic and reversible airway constriction and inflammation.

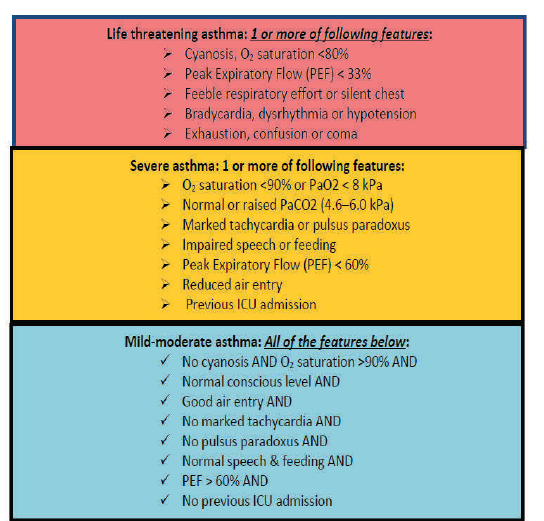
SEVERE ASTHMA IN CHILDREN
Refer to Severe asthma protocol in emergency chapter
MILD TO MODERATE ASTHMA IN CHILDREN

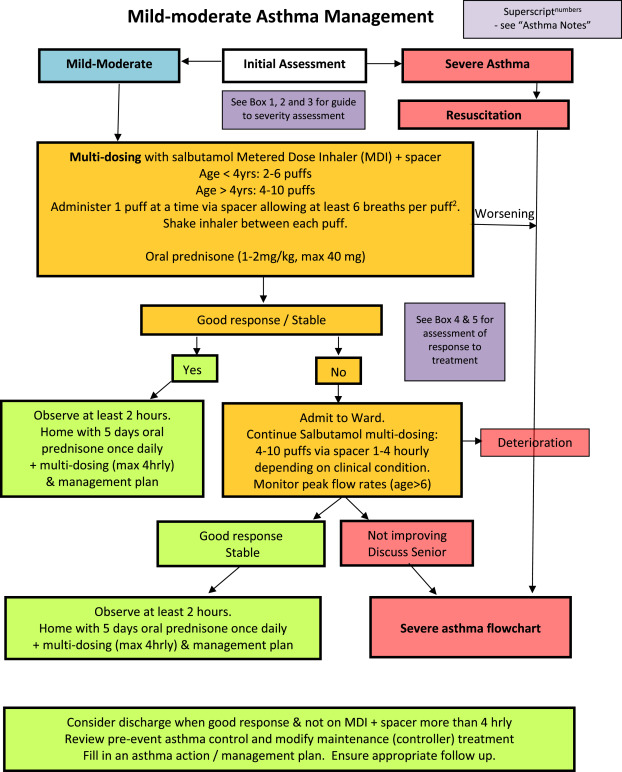
Long term management of asthma in children
- Assess level of asthma Control
|
Assessment of symptom control |
Level of Asthma Control |
|
|
|
In past 4 weeks, has the patient had: • daytime symptoms more than twice a week • Any night waking due to asthma • SABA reliever needed more than twice a week? • Any activity limitation due to asthma? |
|
|
|
|
Well Controlled |
Partly controlled |
Uncontrolled |
|
|
None of these |
1 - 2 of these |
3-4 of these |
|
2. Asthma treatment strategy
GUARDIAN EDUCATION
- How and when to take inhalers (this will need to be observed)
- How to use a spacer
- When to seek help (e.g., breathlessness not controlled by inhalers, sudden increase in the need for 'relievers')
- Possible precipitating factors
- Follow up monthly
Note:
- Use for the shortest time possible before reverting to preferred Agent
- Exercise induced asthma is usually a sign of poor control. If possible, introduce an extra level of medication according to the stepwise approach above
- If asthma is brought on by exercise, older children and adults can take 2 puffs of Salbutamol inhaler via a spacer device 30-60 minutes before games or sports
