- Prior history of ulceration, amputation, Charcot foot, angioplasty or vascular surgery, cigarette smoking, retinopathy.
- Current symptoms of neuropathy (pain, burning, numbness) and vascular disease (fatigue, claudication).
5.4 Diabetic Foot
exp date isn't null, but text field is
- Most common cause of non-traumatic amputation is diabetic foot, which is preventable and treatable.
- Comprehensive foot evaluation should be done initially and at least annually to identify risk factors for ulcers and amputations.
- Individuals with sensory loss or prior ulceration or amputation should have their feet examined at every visit.
- Inspection of the skin
- Assessment of foot deformities
- Neurological assessment: 10-g monofilament testing with at least one other assessment: pinprick, temperature, vibration
- Vascular assessment: pulses in the legs and feet. With symptoms of claudication or decreased or absent pedal pulses: ankle-brachial index, further vascular assessment as appropriate e.g. doppler study.
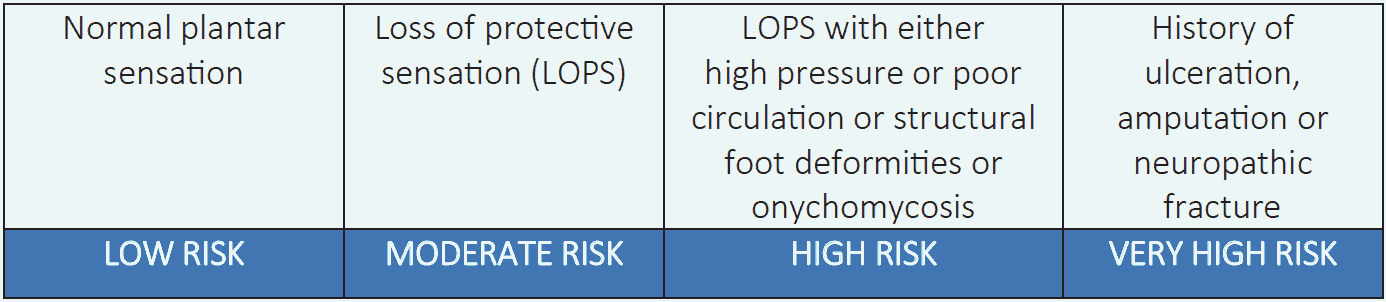
Table 5.3 Risk categories of diabetic foot:5
- A multidisciplinary approach is recommended.
- Provide general preventive foot self-care education to all individuals with diabetes.
- Specialized therapeutic footwear is recommended for high-risk persons with diabetes including those with severe neuropathy, foot deformities, or history of amputation.
Do’s and don’ts for people at risk of diabetic foot
Do’s
- Check feet daily for cuts, blisters, colour changes, swelling, ingrown toe nails. Use a mirror or take someone’s help if required
- Always protect feet with appropriate footwear
- Before wearing shoes check inside for nails, stones or any other sharp object
- Wear socks with shoes; use cotton socks
- Wash socks daily; make sure they have no holes
- Buy new shoes at the end of the day
- After washing, dry feet carefully especially between toes
- Cut nails straight across and file the sharp edges
- Annual foot examination by healthcare professional
Don’ts
- Avoid barefoot walking
- Avoid tight or torn shoes with rough and uneven edges
- Avoid shoes with narrow toe box, high heels or footwear that have no back supports
- Don’t use socks with tight top or rough sim
- Don’t use hot water to wash feet
- Don’t let the feet dry and cracked
- Don’t use corn medicine or blades to remove it by self
- History of prior lower-extremity complications
- Loss of protective sensation
- Structural abnormalities of foot
- Peripheral arterial disease
- Presence of ulcer, gangrene or infection
